1.Clinical practice guidelines
for Achilles tendonitis

Does Achilles tendinitis really have to be inflamed?
Risk factors: abnormal range of motion of the dorsiflexor joint of the ankle, abnormal range of motion of the subtalar joint, decreased plantar flexion strength of the ankle, increased varus, and structural abnormalities of the Achilles tendon as intrinsic risk factors for Achilles tendon pathology. At the same time will be obese, High blood pressure, hyperlipidemia and diabetes as and Achilles tendon Pathology associated with physical conditions. will train errors, Environmental factors, equipment defects as Achilles tendon pathology extrinsic risk factors.
Interventions: eccentric training, low-level laser therapy, iontophoresis, stretching, foot brace, manual therapy, taping, heel elevation, night splinting. Studies have shown that only eccentric training has strong evidence to support its effectiveness when used alone, and no other interventions have strong evidence of efficacy alone. Clinically, it is recommended to choose appropriate interventions according to the actual conditions and needs of patients.
2. Detailed
introduction of heel pain interventions
Anti-inflammatory drugs: examination of the plantar fascial tissue removed by surgery found no inflammatory features, so especially chronic plantar fasciitis may be more appropriate to call plantar fascial disease, and clinically recommended for acute heel pain patients can use ice and anti-inflammatory intervention, for chronic heel pain patients, through micro-inflammatory response to promote tissue repair and reorganization is one of the rehabilitation methods.
Manual therapy: soft tissue release & joint loosening & therapeutic exercises = effective reduction of symptoms & dysfunction in patients with heel pain
Night splints: Night splints are recommended for patients who have pain in the first step of waking up in the morning for 1 to 3 months. Pay attention to keep the dorsiflexion of the foot and the dorsiflexion of the first metatarsophalangeal joint.
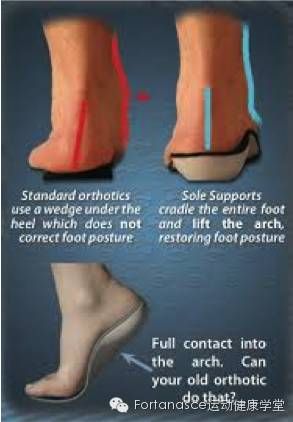
Insoles: Use insoles to support the arch, cushion the heel, and use short-term (2 weeks) to long-term (1 year) to relieve pain and improve function. This is especially true in patients who respond to anti-pronatal taping.
Patching: Anti-pronator banding relieves acute pain (within 3 weeks) and improves function. Elastic patches can also be used to relieve pain in the short term (1 week) by attaching the gastrocnemius muscle and plantar fascia.
Stretching: stretching the plantar fascia and gastrocnemius/soleus muscle provides short-term (1 week to 4 months) pain relief. Heel pads can be used to help enhance stretching.
Physical factors: ultrasound is not recommended; It is recommended to use manipulation, stretching, and insoles instead of electrotherapy to improve the medium- to long-term (1-6 months) effect; Ultrabiotically introduced ketoprofen gels can be used.
Weight Loss Education and Counseling: To help patients achieve or maintain optimal lean body mass, exercise programs are recommended, and professionals are recommended to address nutritional issues.
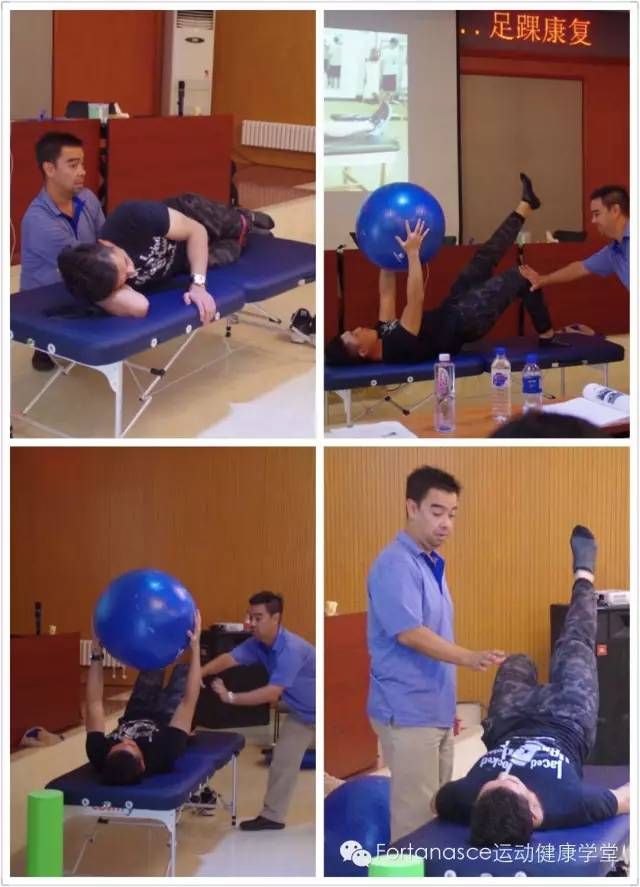
Therapeutic exercises and neuromuscular reeducation: Therapeutic exercises enhance pronation control and absorption of external forces during weight-bearing activities.
Dry needling: studies do not support better results with trigger point dry needling, but dry needling is effective in clinical experience.
(1) Key clinical findings of heel pain/plantar fasciitis:
• Plantar heel pain: most pronounced at first few steps after a period of immobilization, and worsens after prolonged weight bearing (chief complaint)
• A recent increase in weight-bearing activity has led to heel pain
• Palpation/irritation of the proximal attachment site of plantar fascia reproduces pain complaining
• The winch tested positive
• Tarsal tunnel test and other lower extremity tone and sensory tests, negative peripheral nerve entrapment
• Lumbar pressure test or other lumbar pelvic region involving or radiating pain, complaints of low back pain, lumbar pelvic band irritation, lower extremity tension, neurological status test negative
(2) Evaluation of functional level, physical injury, measurement of efficacy:
• Complains of efficacy measures, such as the Foot and Ankle Capacity Scale
• VAS, which assesses pain that begins a few steps after a period of immobilization
• Active and passive range of motion from the calf joint dorsiflexion
• Foot gauges
• BMI of non-athletes
•Lower extremity musculoskeletal and biomechanical assessment, including the following gait elements:
– The range of motion and accessory range of motion of the first metatarsophalangeal joint extends 65 degrees in the pre-swing phase
– Hindfoot/heel range of motion and accessory range of motion are valgued 4-6 degrees during the weight-bearing buffer period
– Posttibial muscle strength and motor coordination control the intertarsal joint during the weight-bearing buffer period
– Fibulus longus muscle strength and motor coordination control the intertarsal joint at the end of support
– Dorsiflexion range of motion, accessory range of motion, calf triceps muscle length and tissue range of motion 10 degrees from the calf joint dorsiflexion at the end of support
– Gastrocnemius/soleus muscle strength and motor coordination control tibial anterior movement during mid-support and end-support push
– Knee and thigh muscle flexibility extends 0 degrees at the end of support and 60 degrees at the beginning of swing
– Quadriceps strength and motor coordination control knee flexion during stress response
– Hip range of motion and muscle flexibility are extended 10 degrees at the end of support
– Trunk, hip and thigh strength and motor coordination control of lower extremity internal rotation during weight-bearing response and hip abduction during weight-bearing response and mid-support
(3) Intervention – direct treatment of plantar fascia-related injuries
• Therapeutic exercises – plantar fascial stretching – gastrocnemius/soleus muscle stretching
• Manual therapy
– Joint loosening improves the limitation of range of motion of the lower extremities, focusing on improving dorsiflexion of the calf joint-plantar fascial soft tissue release
– Soft-tissue release of myofascia of gastrocnemius and soleibut, especially at mixer points and soft tissue restricted areas
• Tapping – Taping against pronation
• Patient education and counseling
– Address/discuss strategies to improve weight bearing at work, leisure or daily life
– Address/discuss the choice of shoes that relieve the usual heavy stress
– Address/discuss obtaining or maintaining optimal lean body mass, especially in non-athlete populations with high BMI
•insole
– Use over-the-counter/prefabricated or custom insoles to support the medial arch and/or cushion the heel, especially in patients with foot shape index showing hypersunation, insufficient lower extremity strength and motor coordination, and/or efficacy of anti-pronator patching
– Use of over-the-counter heel pads, shoes to improve heel cushioning, and/or corrective strategies that include heel cushioning, especially in patients with decreased impact cushioning, hypersunation on foot shape index, and/or concurrent lack of lower extremity strength and motor coordination
• Night splints – when appropriate, use night splints for 1-3 months, depending on the effects of other interventions
• Physical factors – iontophoresis, low-level laser, or ultrasound-introduced therapy for patients with acute pain, who maintain the above interventions, who have reduced pain and can tolerate other treatments
(4) Intervention – directly address heel pain/plantar fasciitis-related lower extremity physical injuries
• Manual therapy
– Loose joints and manual stretching to restore normal range of motion of the first metatarsophalangeal joint, tarsometatarsal joint, talus heel joint, talus calf joint, knee joint, hip joint
-Soft tissue release with manual stretching restores the myofascia of the calves, thighs, and hips, especially at the end of support
• Therapeutic exercises and neuromuscular re-education – Train muscle strength and the ability to control tarsal pronation (posterior tibial and peroneal longus muscles), ankle plantar flexion (tibial anterior muscle), knee flexion (quadriceps), hip adduction (gluteus medius), lower extremity internal rotation (external hip rotator), reduce pronation tendencies, and improve the ability of cushioning to absorb weights
Post time: Jan-12-2023